3. Forms of Urticaria
Spontaneous urticaria is the most common form of urticaria. One in four people develop spontaneous urticaria in the course of their lives. The key characteristic is that the symptoms occur “out of the blue”. As a rule, the signs of illness (wheals, itchiness and angioedema) cannot be reproduced on command and triggers and causes responsible cannot be determined upon first sight. Generally spontaneous urticaria lasts only a few days or weeks. It is then defined as acute spontaneous urticaria. For up to 10 % of all patients with spontaneous urticaria, the symptoms last longer than 6 wheals. This is then called a chronic spontaneous urticaria.
3.1.1 Acute spontaneous urticaria
Frank Siebenhaar
Spontaneous acute urticaria involves a one-off episode that lasts a few days or weeks with the unmistakable symptoms and discomforts of urticaria. The clinical picture therefore usually develops within hours or a few days and then slowly abates again. The causes are not always clear. In many cases, however, it is possible to state precisely the circumstance that triggered the symptoms, e.g. an infection and/or the ingestion of pain tablets or other drugs (including those which were previously tolerated well).
In most cases (> 90 %), a spontaneous acute urticaria lasts only a few days to weeks and can be well controlled therapeutically in this period. Treatment of acute urticaria consists primarily in the suppression of symptoms, and in general it is neither necessary nor practical to conduct an intensive search for causes. If it is suspected that the urticaria is due to an allergy, e.g. against food, it may be sensible to undergo an allergology examination. The more decisive factor is to recognise and treat possible complications (shortness of breath or discomfort in swallowing) and to avoid possible triggers to the extent that they are known.
Symptoms
During spontaneous acute urticaria flares, wheals and/or angioedema appear, i.e. the typical symptoms of urticaria. The wheals are accompanied by severe itching and sometimes by burning and pain in the skin, too (Ill. 9).

Illustration 9: Extensive spontaneous urticaria wheals (Source: www.urtikaria.net)
While the wheals appear on all body areas, angioedema (deep swelling in the skin) frequently occurs in the area of the face or on hands and feet or in the genital area.
Serious spontaneous acute urticaria may lead to an elevated body temperature, besides headaches, diarrhoea, breathing difficulties, joint pain, fatigue and exhaustion may occur. It is often not clearly distinguishable whether these symptoms are directly attributable to urticaria or an underlying infection.
Triggers and causes
Among the more common causes of acute urticaria are infections (e.g. of the respiratory tract), drug intolerances (e.g. acetylsalicylic acid, which is contained, among others, in Aspirin® and Thomapyrin®) food allergies/intolerances. By contrast detergents or personal hygiene products such as shampoos, creams or shower gels hardly ever trigger urticaria. Drugs which more frequently trigger urticaria:
- antipyretic pain killers (Acetylsalicylic acid = ASS, Diclofenac, Ibuprofen)
- antibiotics (Penicillin, Cephalosporin)
Principally almost all drugs can trigger spontaneous acute urticaria. An important indicator is a close temporal connection between beginning drug administration and the beginning of the urticaria symptoms. The diagnosis of a drug allergy should be made with great caution as it means that the patient may no longer receive the drug in future.
Examinations
As a rule it is not necessary to carry out extensive examinations or even a complex search for the triggers and causes of a spontaneous acute urticaria. Firstly, in many cases the cause is obvious, for instance when the urticaria appears in the upper respiratory tract during an infection (“Flue”, “Cold”) or after ingesting a drug (e.g. Aspirin®). Secondly, in most cases spontaneous acute urticaria heals within a few days or weeks. Further examinations are only sensible if a true allergic reaction is suspected or another serious underlying disease.
Treatment
Fortunately enough and in most cases it usually only takes a few days before the symptoms of acute urticaria subside on their own. This type of urticaria is therefore only treated symptomatically, i.e. the appearance of wheal, itchiness and/or angioedema is suppressed by drugs, so-called antihistamines (also called allergy medications). Thereby a higher dose may be necessary for some days or weeks. The antihistamines should be taken regularly during this episode and not only optionally as needed. If the bout of spontaneous acute urticaria is severe and is accompanied by angioedema, difficulty in swallowing or respiratory distress, further drugs (such as, for instance, cortisones) should be administered. Locally applied therapeutic substances are of little use. Of course suspected triggers, when and where possible, should be avoided in future.
3.1.2 Spontaneous chronic urticaria
Karoline Krause
Symptoms
As soon as the symptoms of spontaneous urticaria persist for more than 6 weeks, spontaneous chronic urticaria is spoken of. Then the probability starts to decrease that the disease will disappear again in a short time. Urticaria of this type, with wheals and/or angioedema appearing daily, weekly or more seldom, can last for years (and sometimes decades) and can often not be tolerated without the regular administration of drugs. There are many underlying causes for spontaneous urticaria.
Triggers and causes
In the case of severe, therapy resistant and long persisting spontaneous urticaria a thorough search into the triggers and causes is recommended. The aim is to identify them and (in as far as possible) to eliminate them. The reason behind urticaria being caused by many different causes and triggers is that mast cells can be activated by a large number of factors. These triggering factors can be categorised in 3 subgroups.
- auto-reactive urticaria: intolerance to the body’s own substances
- infection urticaria: reactions to chronic focus of infection or inflammation which do not necessarily entail further symptoms, e.g. in the digestive tract
- intolerance-related urticaria; hyper sensitivity to food additives such as colour, aroma or preservative substances and food rich in histamines or so-called histamine liberators. These substances are also found in absolutely natural food.
Drugs can also cause such incompatibility reactions, e.g. acetylsalicylic acid, among others contained in Aspirin® and Thomapyrin® but also other pain killers and drugs against absolutely different symptoms.
About one third of all the cases of spontaneous chronic urticaria can be classified in one of the groups named above. Other causes of spontaneous chronic urticaria, as for instance allergies to food, are very rare. In about one third of the patients no underlying cause can be found despite thorough examination.
Examinations
In every case of a spontaneous chronic urticaria it must first be ascertained that really such a type of urticaria is concerned. Then the severity of the disease and the impairment of life quality should be determined. In addition blood analysis should be made to find out whether there are signs of a severe inflammation. If there is a severe, therapy-resistant and long lasting spontaneous chronic urticaria, underlying causes should be looked for, i.e. a check made whether an auto-reactive urticaria, and infection urticaria or an intolerance urticaria is involved.
Auto-reactive urticaria can be diagnosed quickly and safely using the autologous serum test (ASST=autologous skin serum test). For this purpose the fresh full blood serum obtained is injected in the skin of the patient in a type of allergy test. If a wheal appears on this spot, this indicates that the patient reacts “allergically” to his own serum.
Particularly infections of the gastro intestinal tract caused by helicobacter pylori, an infection in the ear, nose and throat or tooth roots are particularly frequently the cause of infection urticaria. The diagnostics of an infection urticaria concentrate on the search for infections in these areas. The diagnosis of intolerance urticaria is made by a special diet lasting 4 weeks. In patients with intolerance urticaria this leads to a clear improvement all the way to full recovery. Allergy tests are not sensible for this type of food intolerance.
Treatment
Treatment aims at curing spontaneous chronic urticaria. Where possible this should ensue by curing the spontaneous chronic urticaria, i.e. by eliminating the underlying cause. For instance in the case of an infection urticaria the focus should be eliminated and in the case of intolerance urticaria the triggering substances should be avoided. If this kind of curative therapy approach is not possible or is ineffective, symptomatic treatment is administered. The international guideline for chronic urticaria recommends a three-phase therapy plan. The base therapy consists of the ingestion of non-sedating antihistamines, the so-called antihistamine of the 2nd generation. Should no relief of the symptoms be experienced the dose of the antihistamine is increased. If symptoms nevertheless appear, Omalizumab should be administered (antibodies against immune globulin E). Alternatively the immunosuppressant drug Ciclosporine A should be used (suppresses the immune-reaction of the body) or the anti-inflammation drug Montelukast (a leukotriene antagonist) is administered. Advice is explicitly against the ongoing administration of cortisone as extended therapy. Cortisone may only be administered for a few days as short-term therapy when the patient is suffering severe bouts. Cortisone in the form of ointments or creams on the other hand is ineffective when urticaria is involved. Advice is explicitly against this application. The treatment recommendations of the guideline are based on a strictly scientific evaluation of clinical studies. Therefore the experimental treatment processes are not considered in guidelines. Nevertheless the experience gained by many physicians with one or the other alternative treatment method has been good, for instance with auto-blood therapy. However, great care must be taken in general when turning to alternative therapies.
All too often absolutely ineffective or even dangerous forms of therapy are offered at considerable costs. In the case of severe spontaneous chronic urticaria, e.g. when mucous membranes swell accompanied by difficulties in swallowing and respiratory distress, patients should always have an emergency kit at hand to keep serious urticaria episodes under control. Usually such emergency kits contain a fast-acting cortisone preparation and an antihistamine.
This group includes urticaria forms involving wheals, itchiness and/or angioedema which only appear when triggered by specific stimuli. The largest subgroup of physical/inducible urticaria is physical urticaria. The symptoms are triggered by rubbing, cold, heat, pressure and sunlight (i.e. physical stimuli). All forms of inducible urticaria can occur individually, together with one or several other forms of inducible urticaria or even frequently in patients suffering from spontaneous chronic urticaria.
3.2.1 Symptomatic dermographism / Urticaria factitia
Nicole Schoepke
Symptomatic dermographism, often also called urticaria factitia, belongs to the group of physically inducible urticaria and represents the most common sub-form of physical urticaria. It often occurs with other forms of urticaria. The triggering stimulus for itching and/or burning skin and the stripe-like wheals is the impact of shear forces on the skin, which arise, for instance when rubbing, scratching or chafing (Ill. 10, 11).


Illustration 10 a - and b -: Symptomatic dermographism (Urticaria factitia). A few minutes after “writing” the lettering appears as wheal on the skin. Illustration a - directly after “writing”, illustration b 5 minutes later. (Source: Allergy Centre Charité)

Illustration 11a: Symptomatic dermographism (Urticaria factitia) (Source: Allergy Centre Charité)
The frequency of symptomatic dermographism in the general population, depending on the source of literature, amounts to up 5 %. Particularly young adults between the ages of 20 and 30 are affected. The data on the duration fluctuate between 2 and 5 years, whereby these figures are of purely statistical nature and not applicable to individual patients.
Symptoms
As with other forms of urticaria the main symptoms of symptomatic dermographism are temporary wheals, flaring, itchiness and/or burning skin. Less commonly prickling, stinging and heat sensitivity are described. It is important that: the skin manifestations never occur spontaneously but exclusively at such spots at which shearing forces were applied, this means, for instance, areas where tight clothing rubbed against the skin or which were scratched. The strength of the shearing forces required as trigger varies considerably. Some patients report that the symptoms occur after taking a shower. In such cases the shearing force of the water jet or of following drying sufficed to trigger the symptoms. In other cases strong scratching triggers changes of the skin.
The wheals occur within seconds to but a few minutes on patients with symptomatic dermographism and can last up to several hours. The sequence often observed of the skin reaction is, as summarised briefly: After rubbing or scratching the skin it reddens (through increased blood flow) which is followed by the formation of a reddened aureole extending far beyond the trigger spot at which a wheal develops and itching begins. The wheal is initially still red. It then turns whitish and after a few minutes its full clinical picture appears. The symptoms then disappear in the same order as they appeared: The flare fades after a short time and then itchiness subsides and disappears together with the wheal. The wheals are stripe-like or elongated and their shape corresponds to the preceding stimulant on the skin.
Triggers and causes
As a rule no cause can be found for symptomatic dermographism. A medical examination, contrary to the cause of spontaneous chronic urticaria, for the underlying causes is therefore not indicated.
Examinations
Diagnosing dermographic urticaria is relatively simple: most patients are aware that scratching is the trigger for wheals to develop. In the medical examination a wooden spatula or a special instrument with a so-called dermographometer, is stroked across the skin (for instance on the back or forearm) asserting moderate pressure. Almost all people will demonstrate skin reaction, the so-called dermographism (Greek for “writing on the skin”). In the case of healthy people a “red dermographism” which is no more than a short reddening of the skin as reaction to the mechanical stimulation. In patients with symptomatic dermographism, however, wheals develop with the typical itching flare which only disappears latest after several hours without further consequences.
How can the severity of the disease and the effectiveness of the treatment be determined? A dermographometer is used e.g. FricTest® (www.moxie-gmbh.de); this instrument consists of a flat plastic comb with 4 plastic pins of different lengths which are applied vertically to the skin and stroked over the skin under pressure (Ill. 11b). After 10 minutes every single pin is read. The so-called threshold value can be determined, i.e. the slightest shearing force required to trigger a wheal.
Illustration 11 b: b FricTest®, a dermographometer to determine the severity of the symptoms
Treatment
Because so little is known about the causes of dermographism, a causal treatment is not possible. All patients are first and foremost advised to avoid the triggering stimuli in as far as possible. This particularly included avoidance of all tight, pinching and scouring clothing and tight belts, to turn T-shirts “inside out” or to use laundry softeners for towels for instance. Ensure sufficiently rehydrating skin care is used to avoid additional itching from dry skin. What steps should be taken in addition? An attempt is made to completely prevent the occurrence with various drugs, indeed until symptomatic dermographism heals on its own. The most recommended drugs are simple dosing of non-sedating antihistamines (also called “antihistamines of the 2nd generation, for instance Loratadin, Cetirizin …). If symptoms continue to occur the dose can be increased up to the fourfold of the simple daily dose. If this does not lead to sufficient protection either, other drugs, e.g. Omalizumab may be of help. You get the best help from a dermatologist or an allergist.
3.2.2 Pressure urticaria
Markus Magerl
Pressure urticaria is distinguished from symptomatic dermographism. In the case of this rare disease swellings, which are often deep down and may also be painful in joint areas, occur a few hours after application of pressure. The swellings are accompanied by a flare and frequently only disappear after 1 to 2 days. The typically volatile surface wheals, as occurring in other forms of urticaria, are not found.
The pressure required as trigger is relatively high and has to exert pressure to one spot for a longer period of time. Simply scratching the skin cannot trigger pressure urticaria. To confirm suspected pressure urticaria a pressure test is made (Ill. 7). Thereby a 5 kg stamp is placed on the arm or thigh where it remains for 15 minutes. It is read six hours later, should the test result be positive a rough reddened swelling is found where the test took place.

Illustration 7: Pressure stamp test when suspecting pressure urticaria (Source: Allergy Centre Charité)
Treatment of pressure urticaria is a challenge. Antihistamines of the 2nd generation often only help in higher doses. It is not uncommon that other substances have to be taken in addition. There is no generally applicable medicinal therapy recommendation.
Quick help and considerable relief can be achieved by pressure release, which unfortunately cannot be realised in all situations. As pressure is defined as a certain impact of force to on certain surface, there are two possibilities to reduce the pressure. On the one hand an attempt may be made to reduce the force; on the other hand the surface can be extended on which this force has an impact. It is important to wear wide and soft shoes, to use well-padded straps on bags and backpacks and to take similar measures to prevent such skin symptoms from developing. As a whole pressure urticaria is hardly ever a cause which would make a healing treatment possible. As a whole pressure urticaria is a rather rare form of urticaria. It often occurs in combination with a spontaneous chronic urticaria.
3.2.3 Cold urticaria
Marina Abajian
Cold urticaria is one of the more common forms of physical urticaria. As the name already suggests, cold is the trigger for the skin manifestations. “Cold” is to be understood in a very broad sense. Anything that is cooler than the human skin may be considered cold.
Each patient has an own individual threshold temperature. This is the highest temperature which still triggers a wheal. This means temperatures which are elevated above the threshold temperature do not trigger wheals, however all temperatures under the threshold temperature do so. The higher the threshold temperature, the more frequently will the patient have symptoms. In the course of the disease the threshold temperature remains relatively constant; however, it can be lowered by treatment.
Cold allergy or cold urticaria?
The terms “cold urticaria” and “cold allergy” are often used synonymously. It is, however, not quite correct. Cold urticaria does indeed cause allergy-like symptoms, but it is not an allergy in the true sense of the word. An allergy is based on the formation of antibodies against a triggering substance, the allergen. An allergen is actually a harmless substance found in our environment, occasionally also a substance found in the body. An allergic reaction occurs upon contact with the allergen. As cold is not a material no antibodies can be formed against cold, therefore a cold allergy cannot exist. The precise mechanisms on which cold urticaria is based have not been fully understood yet. Presumably the processes taking place in the body as reaction to cold lead indirectly to the activation of mast cells in the skin and to the release of histamine and other inflammatory substances.
Cold urticaria is a common form of physical urticaria. In cold countries (e.g. Scandinavia) it is more common, in warm countries a little less common. Women are affected roughly twice as often as men, both typically in young adulthood in both sexes. The disease lasts on average for 5 to 8 years. In our latitudes the disease is clearly prevalent in winter.
Symptoms
In the case of cold urticaria wheals and/or swelling result from the direct contact of the skin or mucous membranes with cold of no matter what type (air, water, objects, beverages or meals, evaporated sweat). The wheals and swelling sometimes already appear during cold impact, usually however, a few minutes later. They disappear within a few hours. As a rule the skin reactions (wheals, flares, itching, burning, swellings) are limited to the spot of cold impact. Therefor in winter usually the unclothed parts of the body, such as hands and face, are affected. Many patients report that apart from the absolute temperature a quick change in temperature, i.e. a big difference in temperature (transition from warm to cold) may lead to the appearance of wheals.
Complications
Cold urticaria holds particular risks, which fortunately only rarely lead to severe complications. However, in the case of extensive contact with cold, for instance swimming in cold water, it can become dangerous. The literal “plunge into the cold water” can trigger a generalised urticarial reaction involving the whole body which can lead to a shock. Due to the histamine release the blood vessels are expanded and blood pressure drops. Even more fluid is taken from the circulation by the wheal formation which leads to a further drop in the blood pressure. As a result the blood supply to critical organs (like the brain, heart, kidneys) is reduced, which may end in unconsciousness and drowning.
Cold drinks or ice-cream can lead to swelling in the throat area of patients with cold urticaria. Such swelling may not only result in difficulty in swallowing, but also in respiratory distress, or to a complete respiratory obstruction.
Caution is required for cold urticaria patients during hospitalization and particularly during operations because infusion solutions that are not warmed to body temperature prior to intravenous application can trigger serious attacks of cold urticaria. The anaesthesiologist should therefore always be informed about the cold urticaria condition.
Triggers and causes
Cold urticaria usually appears for no known reason, however rarely develops as consequence of another disease. In this connection reports are found in literature on haematology diseases, infection from bacteria, viruses and parasites and preceding insect bites in some cases. It is, however, disputable as to which extent they play a causal role in the development of cold urticaria.
Examinations
Diagnosis of cold urticaria is relatively simple. A test is first made to find out whether cold urticaria is really present. Various tests can be carried out, of which the so-called ice cube test is the most common and simplest test method. Hereby a melting ice cube in a plastic bag is placed on the skin of the forearm for 5 minutes and the formation of the wheals are analysed 10 minutes after the end of the test. A cold urticaria can be diagnosed much more precisely with an electronic testing device, the TempTest® (Ill. 13). Thereby a metal cooling element with a precisely defined temperature curve is applied to the skin. This not only allows for the determination whether cold urticaria is concerned, but also the precise threshold temperature.

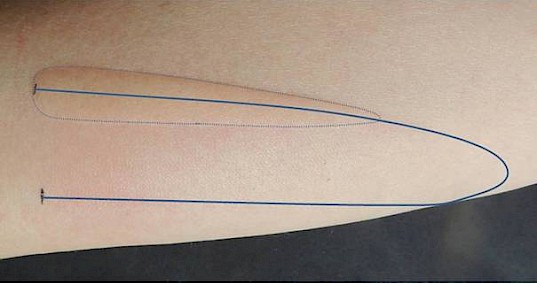
Illustration 13a and b:: TempTest® device for standardised cold provocation of the skin. The TempTest® device makes skin provocation with temperatures for 4oC to 44oC possible. The temperatures are generated with peltier elements at the open ends of the „U“. All temperatures in between develop in the course of the “U“. The skin reaction complies with a certain threshold temperature in its length. A continuous line: Course of the “U“ on the skin during the test. Dotted line: border of the wheal resulting from the cold. (Source: Allergy Centre Charité, www.moxie-gmbh.de)
Why is it of help for cold urticaria patients to know their personal threshold temperatures? It is the threshold temperature which is the skin temperature as from which level symptoms occur. The patient who knows his own threshold temperature can pay attention to protect his skin from this and colder temperatures and to avoid exposing it to such temperatures. Furthermore, the severity of the manifestation can be assessed. The higher the threshold temperature, the higher the activity of the illness is. Furthermore, the success of the therapy can be determined quite well and the best treatment found based on the threshold temperature. In rare cases of cold urticaria the skin does not react to local exposure to cold. In such cases a longer period of provocation or the use of another provocation test (cold bracelet, cold chamber) is sensible.
Treatment
It is of utmost importance that patients with cold urticaria know all about their disease and avoid contact with cold. This includes, among others, wearing thick warm clothing, gloves, caps and scarves in cold temperatures, avoiding taking baths in cold water and avoiding ice-cold food or beverages. Nevertheless, complete avoidance, particularly when threshold temperature is high, is not possible in everyday life. As the causes of the disease are unknown for cold urticaria and as a rule remain unknown, the focus is clearly on the avoidance of symptoms.
Frequently cold urticaria patients are advised to undergo an antibiotics treatment, e.g. with Doxycycline. It may be sensible as the cold urticaria can be cured with it. However, no good studies on this treatment are available so far and it must be assumed that less than half the patients are relieved of their symptoms.
A non-sedative antihistamine should be taken daily (or prior to contact with cold) as protection against the occurrence of wheals, itching and swelling after contact with cold. Some patients have to take higher doses, i.e. two or even four tablets daily, to provide them with sufficient protection. Antihistamines are a protection against the effect of histamine, which is released when the skin of cold urticaria patients comes into contact with cold and which then triggers wheals and itching. (s. Section 1.3 “The mast cell as key cell”). Omalizumab is similarly effective in patients with cold urticaria as in patients with spontaneous chronic urticaria.
However, no explicit approval has been issued for Omalizumab for therapy of cold urticaria.
A further form of cold urticaria patients is the so-called cold desensitization treatment. The sensitivity of the skin to cold is lowered by taking daily cold showers. However, this treatment is complex, not entirely without risk and has to be initiated under inpatient conditions. This means it should not be tackled on one’s own initiative, but must, under all circumstances, be carried out by allergists or dermatologists.
High risk patients should always have an emergency kit on them. An emergency kit usually consists of a cortisone preparation and an antihistamine. Carrying an adrenalin auto-injector along makes sense for severe cases.
3.2.4 Solar urticaria / light urticaria
Karsten Weller
Sun and wheals
Solar urticaria is one of the uncommon forms of physical urticaria. In the case of solar urticaria, the appearance of wheals and itchiness occurs after exposure to light, particularly sunlight. In common language light urticaria is (wrongly) sometimes called “sun allergy”.
Solar urticaria can occur at any age. Possible women are more frequently affected than men, however, little is yet known about the ratio among the sexes and the duration of solar urticaria. Solar urticaria often persists for many years, sometimes decades. Many solar urticaria patients suffer from further forms of urticaria in addition, such as, for instance symptomatic dermographism (urticaria factitia).
Symptoms
Solar urticaria typically begins suddenly in spring or summer. A few seconds or minutes after exposure to light (UVA, UVB or visible light), itchy wheals form on the skin in the areas exposed to the light. In rare cases wheal formation can also first appear several hours after solar exposure. All parts of the skin protected from the light generally remain unaffected. Lightweight clothing does not completely ward off UVA rays and visible light, this means that solar urticaria can also appear on “covered” areas of the body. Once the sun exposure is discontinued, the symptoms often disappear again in one or two hours. Exposure to lower intensity rays may only cause redness or small wheals, therefor it is not always easy to differentiate solar urticaria from other skin reactions triggered by light. If the entire body is exposed to the triggering rays, then serious symptoms like respiratory distress, dizziness or an anaphylactic shock may occur.
Light tests have shown that patients frequently on react to a certain part of the light range, i.e. only to radiation within a specific wavelength. These wavelengths are called action spectra. Some patients with solar urticaria are intolerant to visible light, other only react to, for us invisible, UVA radiation (340–400 nm wavelength) or to UVB radiation (280-320 nm) (Ill. 14a). Occasionally patients react both to visible light and also to UV radiation.
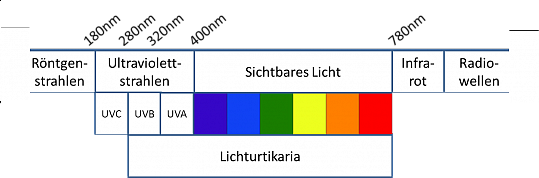
| Röntgenstrahlen | X-rays |
| Infrarot | infrared |
| Ultraviolettstrahlen | ultraviolet rays |
| Sichtbares Licht | visible light |
| Radiowellen | radio waves |
| Lichturtikaria | light/solar urticaria |
Illustration 14a: Wavelength of the light. The symptoms of light urticaria can be triggered by visible light but also by UVA or UVB rays. (Source: Allergy Centre Charité)
It is interesting to note that some patients, whose urticaria is only triggered by the light of the sun, can tolerate artificial light without any problems. For some 70 % of the patients with solar urticaria there is a specific wavelength range, beside the action spectrum, that actually suppresses the formation of wheals. Usually the wavelengths of the inhibition spectrum are longer than those of the action spectrum: If, for instance, the action spectrum is in the UVA range of wavelengths around 320-400 nm, the inhibition spectrum would potential be in visible light (400-780 nm). In most patients with solar urticaria the inhibition of urticaria, however, only occurs if the inhibition spectrum directly follows exposure to the action spectrum.
Potential misidentification
Heat urticaria is a very rare form of physical urticaria, wheals and itchiness occur on patches of skin that are exposed to heat (e.g. warm water or warm air). Therefore heat urticaria, if it occurs in summer, can be confused with solar urticaria. In the case of solar urticaria, as a rule only such areas of the skin are involved which have been exposed to the sun, whereas in the case of heat urticaria the wheals occur more on skin under clothing (heat generation).
To be on the safe side heat and light tests should confirm the diagnoses. Sometime skin changes may also be due to the so-called polymorphous light dermatitis which resembles those of solar urticaria. However, skin changes of polymorphous light dermatitis last much longer (days!). The same applies to photoallergic and phototoxic contact eczema and more rare diseases like lupus erythematosus and porphyria.
Causes
Contrary to the case of spontaneous chronic urticaria, little is known about the possible connection between solar urticaria and infections, food additives, allergies or other causes. Therefore solar urticaria is usually defined as “idiopathic” (= cause not clarified) and as a rule, a search for the cause is not recommended.
Examinations
A light test should be carried out to diagnose solar urticaria. This involves exposing the skin (or parts of the skin) to light of various wavelengths to establish the triggering wavelength range. The test is made with a so-called “photo patch” on patches of the skin not usually exposed to the sun, e.g. on the back or buttocks (Ill. 14b). The light test may also be positive, for other skin diseases triggered by light; i.e. may trigger skin symptoms. However, it is typical for solar urticaria that the wheals appear within a few minutes after radiation on the test areas. These wheals are volatile and almost always subside after 1-2 hours.

Illustration 14b: Wheals after a “UV photo patch“, i.e. a test with various doses of UV light. The patient reacted clearly to UV rays with wheal formation
Treatment
Because it is not exactly known yet how and why solar urticaria occurs, there is currently no known approved effective therapy, which combats the cause of the disease. An attempt is therefore being made to either prevent the urticarial outbreak by protection against light or to alleviate the symptoms.
One relatively simple way to provide protection against exposure to the sun is to use sunscreens with a high light protection factor which filter out a wide range of light, as well to wear appropriate clothing and hats and to primarily stay in the shade. Unfortunately these measures are only effective for patients who react to ultraviolet light, but are of little benefit for urticaria triggered by visible light.
Another option of symptomatic treatment is the administration of antihistamines which block the effects of histamine. Apart from antihistamines all the drugs can be used for treatment which are currently also recommended for spontaneous chronic urticaria.
An alternative therapy that may be successful, but hardly feasible in reality, is a light desensitisation treatment. For this therapy initially only parts of the body, later the whole body, are exposed to light of the triggering wavelengths (phototherapy). The intensive exposure leads to the desensitisation of the skin to light and wheals do not occur so easily. A disadvantage is that the success of this treatment diminishes again when interrupted and continuous light treatments on the other hand, are associated with potential, negative long-term effects.
3.2.5 Cholinergic urticaria
Sabine Altrichter
Cholinergic urticaria is also one of the inducible forms of urticaria. Cholinergic urticaria is also sometimes called “sweat urticaria“, sometimes the term “heat reflex urticaria” is used. In the case of cholinergic urticaria wheals and itchiness occur by an elevation of the body temperature, e.g. by sweating after sports, but also following emotional stress.
Cholinergic urticaria is not an uncommon disease and is one of the more common forms of urticaria. It affects both sexes, indeed particularly young people between the age of 15 and 25. According to a recent study more than one in ten of the 15 to 25-year olds suffer from cholinergic urticaria. According to a study carried out by the Freie Universität Berlin, over one in ten of the 15 to 35-year-olds suffer from cholinergic urticaria. However, only a few people actually discuss the condition with a doctor because in many cases the symptoms are so slight that quality of life is not significantly impaired. This is also confirmed by the observation that only some 0.2 % of the patients at dermatology practices suffer from cholinergic urticaria. Long-term studies have shown that cholinergic urticaria often lasts a long time, on average about 8 years. Some 30 % of those suffering from cholinergic urticaria spend even more than 10 years struggling against it. Fortunately in most cases the severity of the disease abates over time. Some patients report an improvement of their symptoms in summer, which may be related to heat acclimatisation by the body during the warmer seasons.
Cholinergic urticaria, very seldom does occur clustered within families. Interestingly, almost half of all the cholinergic urticaria patients are also congenitally disposed to developing diseases like hay fever, neurodermatitis (so-called “atopic diseases”). Such a connection is not observed in the other forms of urticaria. Cholinergic urticaria occasionally occurs together with spontaneous chronic urticaria.
Symptoms
Cholinergic urticaria often involves the formation of small pinpoint wheals that are typically surrounded by a larger reddened part of the skin. In most cases the skin changes occur within 2 to 20 minutes after the onset of sweating, generally starting on the neck and the upper part of the body. The patient often first notes itchiness or prickliness or burning of the skin. Once the body cools down again, the wheals disappear without a trace within minutes or hours. In mild cases only a few wheals appear, particularly on the upper body. In severe cases the entire body may be affected. Fortunately cholinergic urticaria rarely involves serious symptoms like angioedema (= swellings deep down in the skin), breathing difficulties, nausea, headaches or vascular collapse. Heat and cold urticaria, solar urticaria or even spontaneous chronic urticaria are among the diseases with which cholinergic urticaria can easily be confused, particularly when it is induced by stress. Certain common characteristics are shared by cholinergic urticaria and spontaneous chronic urticaria with exercise-induced anaphylaxis. Exercise-induced anaphylaxis is a mast cell dependent reaction which can lead to an allergic shock after ingesting an allergen (often wheat) in combination with physical exertion. Wheals may also appear. Patients do not suffer any symptoms from exertion alone.
Triggers and causes
Unlike chronic urticaria where the skin changes frequently appear without an external stimulant, cholinergic urticaria symptoms always arise as a result of a trigger. In other words: Cholinergic urticaria patients can bring about an occurrence of the symptoms intentionally. The cholinergic urticaria symptoms are triggered for instance by heat (too thick winter clothing, a hot bath), exertion, eating very spicy food or even by great emotions such as excitement or a scare. Unlike the case of spontaneous chronic urticaria, little is known about the underlying cause of cholinergic urticaria.
Examinations
The most common test procedure to diagnose a cholinergic urticaria is the exertion test (Ill. 15). It is ideally conducted on a stationary bicycle (bike trainer); however, climbing stairs or running is also a possibility. Recently a 30-minute pulse-controlled exertion test has been developed which, apart from providing a diagnosis also makes it possible to determine the degree of severity. In this test a bike provocation is conducted with an increasing pulse rate, up to 170 beats per minute. The time until wheals appears equals the severity of the disease: The quicker the wheals appear, the severer cholinergic urticaria is.

Illustration 15: Typical wheals after exertion test in patients with cholinergic urticaria. (Source: Allergy Centre Charité)
Another option to test for cholinergic urticaria is to take a hot bath or to sit in a sauna. Wheal formation is triggered by the passive warming up. This method is, however only seldom used today because, unlike the test with a bike ergometer the severity of the disease can only be indicated roughly and conducting such a test is more cumbersome.
In urticaria centres skin tests are made in addition. Patients with cholinergic urticaria develop a wheal in the upper skin layer where pricked by the injection when so-called cholinergic substances (e.g. metacholine, acetylcholine or pilocarpine) are injected. Unfortunately the test is frequently falsely negative, this means no wheal arises even though the patient suffers from cholinergic urticaria. This skin test can therefore only be used to confirm a diagnosis. Furthermore, an autologous test sweat-skin-test can be done for which a little inherent sweat of different dilutions is injected in the skin as for an allergy test. It leads to the development of wheals in some patients. This indicates that there is an allergy to an (auto) allergy against inherent sweat.
Are all the tests are negative, although you can be sure you are suffering from cholinergic urticaria? In such a case possibly the tests were carried out in the so-called “refractory time” of the skin. The refractory time is the time after a severe bout of urticaria. The mast cells of the skin are not able to release histamine again in this time. They first have to “recover” to be able to react to stimuli again. It is still not exactly known whether histamine or a yet unknown trigger for mast cell activation (e.g. a neuropeptide or an allergen) is missing in this time. Therefore the exertion tests should not be carried out before at least 24 hours have lapsed since the last bout of cholinergic urticaria.
Treatment
Unfortunately due to the lack of knowledge about the underlying causes of most cases of cholinergic urticaria there is rarely an approach for a causal therapy and thus for a cure. In most cases of cholinergic urticaria recourse to a treatment of the symptoms (symptomatic therapy) has to be made: antihistamines. Modern histamine therapy tops the list for cholinergic urticaria; it prevents histamine from fully effectively triggering the wheal effect. Various preparations have proven to be effective. If a certain antihistamine does not lead to a satisfactory protection, a test may be made as to which of the many other substances available alleviate the symptoms best.
Many patients take antihistamines daily or preventatively before doing sports or other activities which, as experience has shown, produce wheals. Usually one tablet is enough to completely suppress the symptoms. As a whole the therapy of cholinergic urticaria is oriented along the lines of the therapy recommendations in the guidelines for spontaneous chronic urticaria. However cholinergic urticaria has some particularities, which in particular cases also allow variations from therapy recommendations to be successful:
- Ketotifen: Ketotifen is both an antihistamine and also a mast cell stabiliser. In some cases it revealed a good effect in connection with cholinergic urticaria, even in patients who do not respond to other antihistamines. Due to the sedative effect ketotifen is, however, a second option drug and should only be administered in exceptional cases.
- Anticholinergics: Clidinium bromide and butylscopolamine bromide were successfully used for cholinergic urticaria. These drugs lead to reduced sweat production, flares, bloating, disturbed vision, palpitation (tachycardia) and a dry mouth may occur as unwanted side effects. Long-term surveys or studies with a greater number of patients are not available for this drug.
- Other drugs: In individual cases successful therapy was described using propranolol (Beta-Blocker), maprotiline (tetracyclic antidepressant with antihistaminic effect) and chlordiazepoxide (benzodiazepine). However, studies with a greater number of patients would have to be carried out to evaluate the therapeutic benefit of these.
- Hardening – Making use of the refractory time: a further option to get the cholinergic urticaria symptoms under control is to exploit the refraction time, i.e. the time in which the mast cells cannot release histamine. Some patients take advantage of this condition by triggering a controlled bout of urticaria (e.g. by physical exercise) to then be wheal-free for 24 hours. Regular and underlying physical exertion (i.e. without giving rise to symptoms) is better. Therefore if this form of therapy is carried out like a small daily fitness program; the occurrence of severe bouts of wheals can be prevented.
3.2.6 Other forms of urticaria
These include the rare vibration induced angioedema, involving deep swellings triggered by vibrations on the skin, contact urticaria involving wheals which exclusively occur after skin contact with certain substances, e.g. food and aquagenic urticaria involving wheals and itching triggered by skin contact with water. Some of these forms are so seldom that many dermatologists never see a patient with such a form of urticaria during their working lives.
Back to overview.



 English
English Deutsch
Deutsch Francais
Francais Español
Español